What is vicarious trauma?
It is different from empathy, which is relating to and understanding others’ experiences and responses in a compassionate and thoughtful way. It is borne out of a commitment to the people being served and a determination to help ease their suffering. When such committed people feel like they cannot meet that need, and outlets are limited with minimal or ineffective support, they can begin to feel overwhelmed, burdened, resentful and lose hope. It can occur in anyone who works or interacts with people in pain, those in desperate situations or those who need ongoing support after experiencing traumatic events, including healthcare professionals, volunteers and carers.
Many factors can contribute to vicarious trauma, such as lack of safety, cultural factors, inadequate training, minimal support, unrelenting workloads, continued exposure to traumatic material or even personal circumstances and trauma history. In some more rural and remote communities, unique challenges can also increase the risk of vicarious trauma. There is limited access to resources in smaller communities, which can make confidentiality and boundaries more difficult. In some areas, there is a lack of trained health workers attuned to cultural sensitivity and awareness.

Signs and Symptoms
- Feeling off, like you can’t connect to others or feel good about yourself – it can feel like you’re playing a part in a play and not being “in” your life
- Personality changes – feeling mean or cynical
- Misplaced guilt at your own good fortune
- Feeling like your emotions are out of control
- Relationship problems
- Physical issues
- aches and pains
- getting ill more often
- being more clumsy
- Difficulty making good decisions
- A feeling of disconnection to what is important and a loss of meaning and hope in life
- Difficulty managing boundaries – taking on too much, feeling responsible for things that our not your responsibility, taking on other’s problems as your own.
- Increasing substance use or commencing substance use (taking up smoking).
This information has been designed for health professionals
Donate via PAYPAL Today
Related Links
How to go about seeking help
FOLLOWING AN EVENT
HELPFUL TIPS
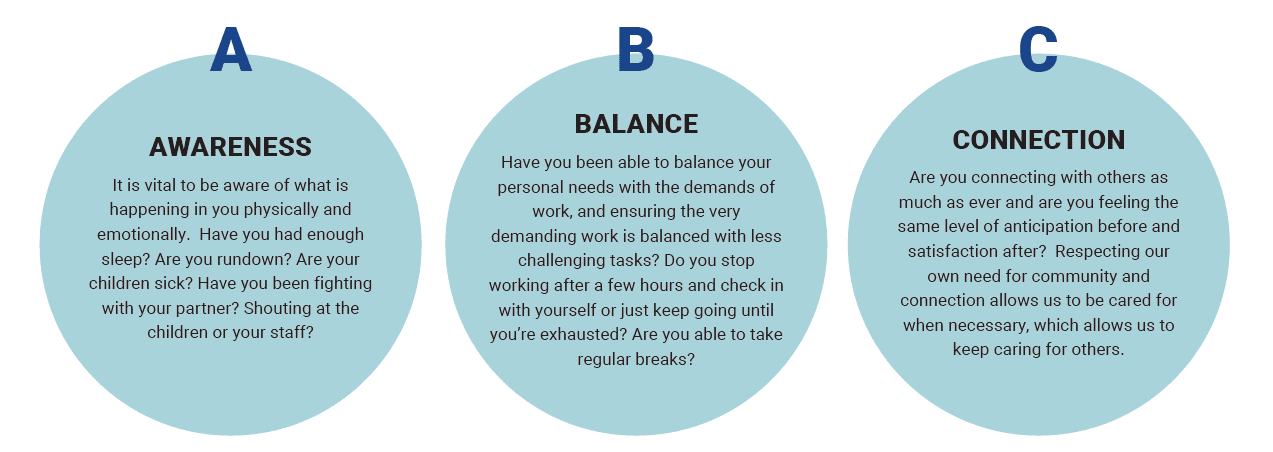
- Self-care is important for all of us, especially if we are in the health professions. It’s not just about soothing activities; it’s about creating a plan or routine that will help you focus, make decisions and stay healthy. Ongoing cultivation of well-being is vital to our health, vitality and quality of life. Diminished clinician wellbeing also puts our patients/clients at more risk as they may be exposed to secondary trauma of the clinician.
- We need to recognise our signs of stress, identify our barriers for seeking out some self-care and see what recharges us and instil those practices and ideas into our daily or weekly lives.
- Time out – make sure to take time for yourself unrelated to work – physically or mentally. Read books, listen to podcasts (note; not related to trauma), and talk to friends about things other than work. Mindfulness apps, and mood-tracking apps like Woebot are good ways to monitor your mood over time to see if this is changing subtly, beneath your consciousness.
- Limit exposure to news and unhelpful social media sites
- Rest – allow yourself to do things without expectation (non-goal-directed activity). Go for a walk without a destination, nap during the day, sip a cup of tea mindfully, it doesn’t need to be big, planned things. Pause and find some mindful moments in the day.
- Play – Look at your current activities and decide which are nurturing and which are depleting e.g., reading to your children might feel nurturing, while cleaning may not feel nurturing. Be sure to do more of the nurturing activities than depleting ones. Sing/hum and dance and get the vagus nerve activated which reduces bodily stress and calms the whole sympathetic nervous system down.
- Be honest – sometimes people helping others feel they must meet every need presented. If you start feeling dread, discomfort, despair or annoyance this needs to be respected as a sign that you may start to be experiencing trauma.
- Discuss with work about getting some further training eg trauma informed care
- Try to avoid taking on direct responsibility for the well-being of trauma survivors with whom you work or support while providing them with the tools they need to care for themselves.
- Set boundaries and say no sometimes. Be aware of your own levels of exhaustion and attend to those.
- Find some time to exercise
- De-brief with colleagues or trusted friends
- Say 3 things you are grateful for in the morning or at night time as it sets up the brain to appreciate the little things which can b useful when life seems overwhelming
Where to FIND SUPPORT
- Peer supervision – the process of reflection on your experience in a safe and respectful way can help us process and contextualise the discomfort experienced
- Speak to your GP – perhaps ask for a Mental health Care Plan to allow you to speak to a professional about your experience
- Phone counselling service
- Peer support through online forums may normalise your experience.
- Consult with a psychologist or other mental health clinician
- For rural and remote workers: Crana Call-1800-805-391

