Triger Warning: this conversation discusses lack of postnatal care, postpartum depression, ptsd, and birth trauma. If you are triggered by these topics you may wish to skip this blog or read it once you have support available. If you are seeking support for your birth trauma, you may wish to join our Facebook Page and contact our Peer Support Service.
Finding Your Tribe
‘Your bloods are completely fine; you don’t need to come back.’ That’s what my GP told me. I was at home with a 2-month-old and struggling. I went to 3 or 4 different GPs, and none of them had a follow-up plan for me when I told them I was depressed and needed help after the birth of my first child.’
I spoke with Tammy when she was in early labour with her second baby. Unfortunately, her experience of postnatal care after a traumatic birth is too common. There will be an age gap of five years between her children. ‘It took me 3 to 4 years before I could even talk about it. I couldn’t get back to the hospital to debrief about my last birth until I was pregnant again.’
In Australia – as in much of the world – postnatal care is the neglected sibling of antenatal and birthing care. Many women are not even aware they need a separate GP appointment for themselves and their baby at six weeks of age. And for some like Tammy, the symptoms of a traumatic birth don’t arise until after that 6-week postnatal check. ‘There are services for young Mums, but what about us who need help and aren’t young? Just because I’m 27, it doesn’t mean I know what the hell I’m doing!’
Mental health a priority
Maternal mental health is a global health priority. In Australia, 10-15% of pregnant women or new mothers experience unaddressed mental health issues. This can lead to anxiety and depression, poor self-esteem, reduced access to antenatal care, decreased maternal-infant attachment, difficulty establishing breastfeeding, intrusive thoughts or images of the birth, fear of future pregnancies and ongoing psychological symptoms later in life.
For some women, their experience of birth trauma may also impact their relationships with others, particularly their intimate partners. Many mums know that something’s not right but don’t always know where to go for help or how to navigate our medical system. Some are reluctant to seek help due to feeling an overwhelming sense of guilt, shame or failure. Others find it hard to speak about the unspeakable: I want to love my baby, but I don’t know how. I’m scared of you, what you did to my body and how you’ve changed my life.
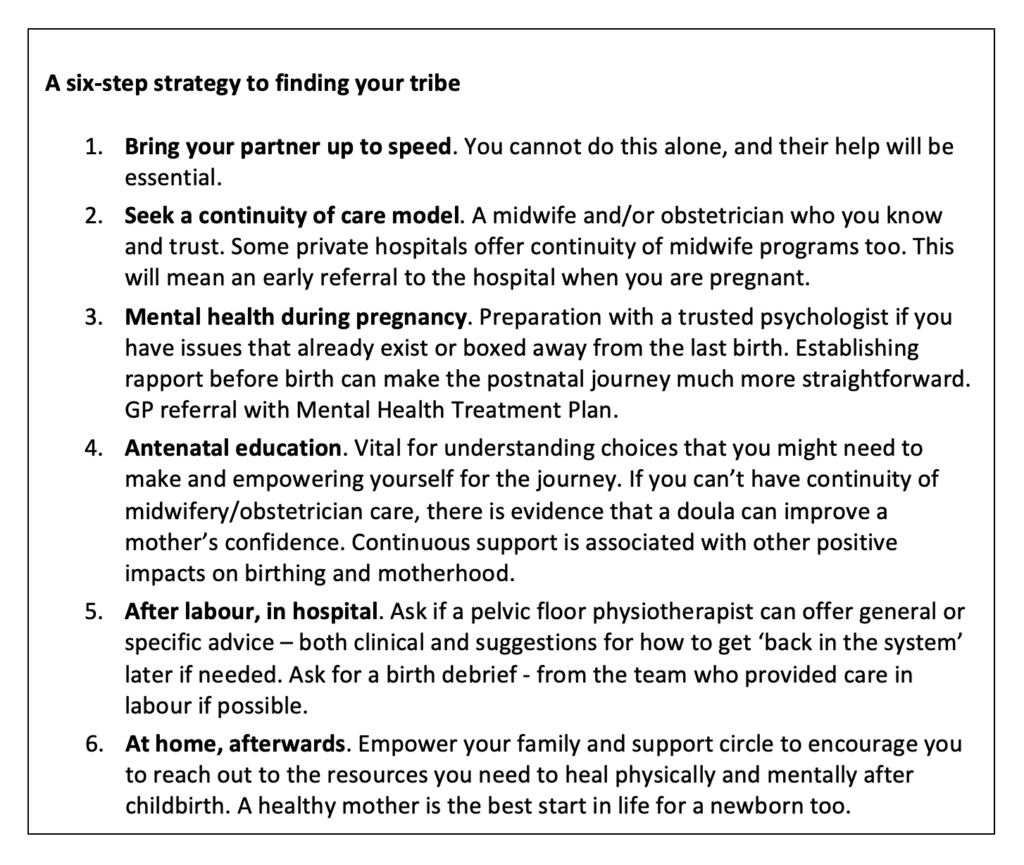
So, who are the tribe that can be there for you? A trusted GP, midwives, obstetricians, perinatal psychologists, psychiatrists and women’s health physiotherapists. These are professionals who will understand what you’ve been through and who have the skills, resources and strategies to help you recover to complete physical and mental health. For Tammy, this might have started with an early debrief after her birth with an obstetrician or midwife, discussing implications for next time, a psychological assessment and therapy sessions if needed.
Accessing services
Accessing the right services sometimes means you need to see your GP with a clear idea of what you want. You can access a psychologist with experience in birth trauma through a GP referral and Mental Health Treatment Plan. Twenty Medicare-rebated sessions are available per calendar year. Many psychologists offer telehealth therapy, which can help when leaving home is difficult. Specialist women’s health physiotherapists practice in larger public hospitals and private practice.
Tammy’s tribe has included her husband, her midwifery group practice (MGP) midwife and peer support through social media. ‘Coming into hospital for induction of labour, I was quite anxious, but having my midwife who can speak for me and who knows what I want has helped so much.’ National guidelines strongly recommend both continuity of care/carer models and collaborative practice by health professionals involved in maternity care.
For now, finding the elusive tribe to help you when you most need it can be a challenge, but the importance of postnatal care is beginning to improve. The Australian Commission on Safety and Quality in Health Care sets expected standards against which all health services in Australia are audited. This year saw the release of a Clinical Care Standard relating to best practice for severe perineal tears during childbirth.
The health professionals listed in this article are key providers for the holistic care of women who experience birth trauma in Australia. Peer support is available through ABTA’s Peer2Peer Support Program.
Tammy’s first baby was born by caesarean, but she achieved a vaginal birth this time. She told me that the actual way Oliver was born wasn’t most important. ‘I was much more supported, in control and empowered this time. That made this a healing birth for me.’
There is a better way, and change has begun.
Dr Danny Tucker, Obstetrician
www.ourmotherhood.com
Instagram.com/ourmotherhood.ig
Melissa Freestun, Psychologist
www.self-psychology.com.au
Instagram.com/_selfpsychology